Irresponsible drug abuse can have many physical, psychological, and behavioural ramifications.
The nature and extent of these consequences depend on several factors, including the drug of choice, the duration of abuse and the method of administration.
Frequent abuse may lead to addiction, a disease whereby one’s brain becomes dependent on the drug.
Drug dependence makes it incredibly difficult to refrain from using and typically precipitates a range of negative long-term health effects.

In addition to lasting direct effects, persistent drug abuse can lead to a number of indirect effects that can seriously impact an individual’s quality of life.
For instance, people may fail to meet familial responsibilities, get in trouble with the law, or experience considerable financial difficulty.
Naturally, the harmful effects of drug abuse impact both general health and life expectancy.
Some studies suggest that people who are addicted to narcotics like heroin may live up to 15 years less than their non-drug-addicted counterparts.
Below we take a comprehensive deep-dive into the long-term health effects of some of the most commonly abused addictive drugs.
To learn more about the impact substance abuse can have on your life and what can be done to stop it, call us on 0800 140 4690

Most people generally don’t think of alcohol as a drug at all.
However, when you consider alcohol’s effects on the individual on top of its effects on other people, it may well be the most harmful drug of abuse there is.
It is estimated that 6% of all global deaths can be attributed to alcohol consumption.
Alcohol abuse is typically characterised by inappropriate consumption that causes harm to the individual, other people, or both.
Consumption of alcohol can lead to addiction and the development of alcohol-use disorder, a condition where people struggle to contain cravings and continue to drink despite its many damaging consequences.

Given the widespread and increasing prevalence of alcohol use across the globe, it is perhaps no surprise to see a growing scientific interest in the relationship between alcohol life expectancy.
Alcohol abuse is associated with a range of long-term physical and psychological effects.
These may include:

The relationship between alcohol and hypertension has now been well-established in the scientific literature. People who regularly drink alcohol are more likely to have high blood pressure.
Additionally, there is a direct relationship between alcohol consumption and blood pressure.
This means that the more you consume, the higher your blood pressure will be. Approximately 16% of people who have high blood pressure have it as a direct consequence of their alcohol use.
A study conducted in China found that men who drank more than 30 units per week were twice as likely as non-drinkers to have isolated systolic hypertension, isolated diastolic hypertension, or combined systolic and diastolic hypertension.
Interestingly, drinking alcohol on an empty stomach appears to increase one’s risk of becoming hypertensive.
One study found that the risk of becoming hypertensive increased by up to 64% for people who consumed alcohol without food.
The type of alcohol consumed bears little significance when it comes to the likelihood of becoming hypertensive. Additionally, the often-reported attenuating effects of red wine on hypertension have yet to receive adequate scientific support.

Drinking alcohol is the leading cause of a specific disease of the heart muscles called alcoholic cardiomyopathy (ACM) across all genders and races.
People with ACM have dilated left ventricles, a reduction in the thickness of left ventricle walls, and an increase in overall left ventricle mass.
It is possible for people to have symptom-free alcoholic cardiomyopathy.
People with asymptomatic ACM consume on average 90 grams of alcohol per day for 5 years.
In comparison, symptomatic alcoholic cardiomyopathy is more likely to occur in people who consume a similar amount of alcohol, but over a period of on average 15 years.
Long-term consumption of large quantities of alcohol is the second leading cause of dilated cardiomyopathy. Expectedly, the prevalence of dilated cardiomyopathy is much higher in alcoholics than it is in the general population.
Therefore, it seems as though the duration of heavy alcohol consumption is more significant than the quantity of alcohol consumed in regard to heart failure.
Alcohol abuse can also cause an irregular heartbeat rhythm called atrial fibrillation.
Atrial fibrillation most typically occurs in the aftermath of a heavy drinking binge, in what’s often referred to as “holiday heart syndrome”. However, consistent consumption of modest amounts of alcohol can also increase the risk of developing atrial fibrillation.
Consumption of more than 14 standard drinks per week may increase the risk of atrial fibrillation by 17% in women. Similarly, consumption of more than 21 standard drinks can increase the risk of atrial fibrillation by 25% in men.
The risk of developing atrial fibrillation may be a more serious consequence of regular heavy consumption than hypertension or obesity.

Consuming more than 2 standard drinks a day may increase the risk of stroke by up to 34%, a risk increase similar to that typically associated with high blood pressure and diabetes.
An analysis of 35 studies investigating the relationship between alcohol consumption and stroke found that heavy consumption increases the likelihood of developing both ischaemic and hemorrhagic stroke.
The implications of this finding are far-reaching considering the significant percentage of stroke survivors who become either permanently disabled or placed in an institution to receive full-time care.
Notably, the type of alcohol consumed does not impact the risk of stroke.

The majority of consumed alcohol is processed by the liver, which means that it is particularly vulnerable to serious damage.
It is estimated that between 20 and 30% of people who abuse alcohol develop liver damage.
Heavy drinkers or people who have received a diagnosis of alcohol use disorder are more likely to develop alcohol liver disease.
Alcohol liver disease is typically characterised by inflammation, scarring called cirrhosis and increased amounts of fat in the liver.
People with alcohol-use disorders are most likely to die from alcohol liver disease and liver cirrhosis.

Consumption of alcohol, excess consumption, in particular, can cause considerable, serious damage to the brain.
For example, chronic consumers of alcohol may see a 22% reduction in the number of neurons located in the frontal cortex compared to non-addicted counterparts.
People with an addiction to alcohol also have significantly lighter brains due to loss of grey and white matter in areas of the brain responsible for information processing and transfer.
Heavy drinkers also have reduced grey and white matter in the cerebellum or, “small brain”, an area at the back of the brain that is responsible for the coordination of voluntary movements.
Excessive consumption of alcohol can also lead to a deficiency in thiamin, or vitamin B1, and cause a preventable memory disorder called Korsakoffs syndrome.

Korsakoffs syndrome is typically characterised by confusion, impaired muscle control, deteriorated coordination, involuntary eye movements, and paralysis of the muscles that control eye movements.
Korsakoffs syndrome, which also seriously affects both semantic and episodic memory, is more often diagnosed after a person has died.
The prevalence of Korsakoffs syndrome is between 1% and 2% for the general population, compared to 12% and 14% in people who have misused alcohol.

The number of people who drink alcohol is steadily on the rise, as is the amount of alcohol being consumed.
In general, people are unaware of the cancer risk associated with the consumption of alcohol.
However, we now know that drinking alcohol is one of the most important risk factors for cancer.
Heavy alcohol consumption increases the risk of one of the most common types of liver cancer called hepatocellular carcinoma.
A meta-analysis of alcohol consumption and the risk of 18 diseases showed that heavy drinkers are almost twice as likely to develop liver cancer.

Alcohol consumption is also a risk factor for breast cancer. Meta-analyses have reported up to a 1.6 times increase in risk for people drinking three drinks a day compared with non-drinkers.
A review of 53 epidemiological studies which involved almost 60,000 patients with breast cancer reported an increased risk of just over 7% for every additional 10 grams of alcohol consumed a day.
Alcohol has also been associated with cancers of the oral cavity, pharynx, oesophagus, and colon, however evidence of the risks associated has thus far been inconsistent.
Find your ideal alcohol rehab by talking to our experts on 0800 140 4690

Opioids are a category of drugs used in a medical context to relieve pain, make people feel relaxed and induce anaesthesia.
The term opiate is used to describe opioids that are derived naturally from the opium poppy plant, while other opioids are synthetically produced.
Examples of opiates:
Examples of well-known synthetic opioids:
Opioids are highly addictive, irrespective of whether they are medically prescribed or used illicitly.
Regular use of opioids can lead to tolerance and dependence.
Developing a tolerance means that people require increasing quantities of the drug taken at more frequent intervals to bring about the desired effect. Eventually, tolerance can manifest as an addiction, which is referred to medically as an opioid use disorder.
Opioid use disorder can lead to a range of long-term medical complications, which may include:

Using illicit opioids like heroin or fentanyl, or misusing prescribed opioid medications such as oxycontin can cause slow and ineffective breathing.
A person may stop breathing altogether in what is known as fatal apnea if they take a large enough dose of an opioid, take opioids along with other types of drugs, or if they have an underlying disease.
Opioids stimulate specific brain receptors found in the brainstem called Mu and delta-opioid receptors which are involved in the regulation of breathing.
The depressant effects of opioids on respiration are caused by an increase in the amount of carbon dioxide present in the bloodstream and a simultaneous decrease in the amount of air that enters and leaves the lungs.
Although opioid-induced respiratory depression can cause death, it can be reliably reversed by an opioid receptor antagonist called naloxone (Narcan).
Naloxone blocks the effects of opioids and is very efficacious in terms of preventing death from an opioid overdose.
Long-term effects of opioid abuse may include:

Like alcohol abuse, opioid use is an independent risk factor for the development of atrial fibrillation.
It is understood that the development of atrial fibrillation is a consequence of sleep-disordered breathing that often accompanies opioid abuse.
Opioid abuse can also cause a potentially life-threatening heart condition called endocarditis, where the inner lining of the heart’s chambers and valves become dangerously inflamed.
Postmortem studies on people who died from an opioid overdose have reported a five-fold increase in the number of inflammatory cells in the cardiac muscle.
Prescription opioid use may increase the risk of developing coronary heart disease and has been associated with an increased risk of cardiovascular death.
Interestingly, women seem to be at a higher risk of cardiovascular death and coronary heart disease than men.
A study comparing arthritis patients treated with opioids or nonsteroidal anti-inflammatory drugs found that opioid-treated patients were twice as likely to sustain a heart attack, five times more likely to require a procedure to unblock coronary arteries, and had almost two times the risk of out-of-hospital cardiac death.

The abuse of opioids has also been associated with diseases of the airways and lungs.
Opioids can cause a tightening of the airway muscles.
This tightening can have a narrowing effect and ultimately obstructs the movement of air in and out of the lungs.
Opioids can also impair the function of immune cells by increasing the release of a chemical called histamine, which may cause airways to go into spasm.
There is evidence to suggest that the chronic use of opioids may worsen pre-existing airway diseases such as asthma.
In particular, patients who snort, smoke, or inject heroin are at a greater risk of asthma exacerbations than those who do not use opioids.

Chronic use of opioids can also increase the risk of developing pneumonia, an infection that causes air sacs in the lungs to become inflamed.
One study showed that morphine specifically can compromise the function of white blood cells called neutrophils and macrophages that fight bacterial and fungal infections in the lungs.

At present in the United States, 1 in 6 women and 1 in 9 men of reproductive age are being prescribed opioid medications every year.
Considering the extensive prescribing of these medications, it is critically important to have an awareness of their potential effects on fertility and pregnancy outcomes.
Studies investigating fertility-related outcomes in women have reported a lower chance of becoming pregnant and an elevated risk of infertility.
Studies have also shown decreased levels of reproductive hormones in both male and female users of opioids.
The use of prescription opioids long-term has also been associated with an absence of menstruation, called amenorrhea, or infrequent menstrual periods, called oligomenorrhea, among people of reproductive age.

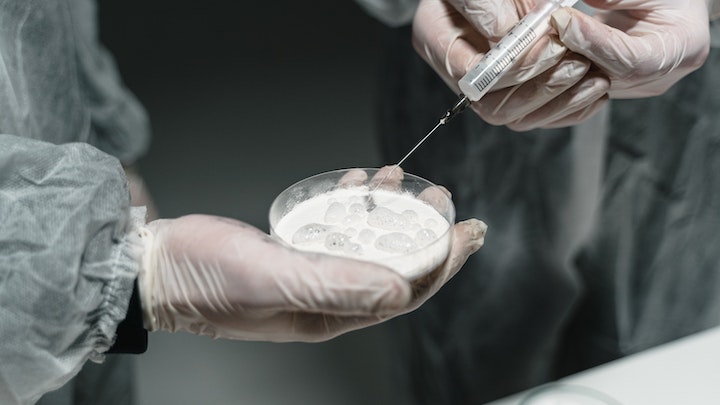
One potentially fatal consequence of opioid abuse is the increased incidence of blood-borne infections, such as hepatitis C, hepatitis B, and human immunodeficiency virus (HIV).
These infections are spread mostly through the use and sharing of contaminated syringes, dirty conditions, and low levels of protective vaccination among opioid abusers.

As mentioned above, the central role of the liver in drug metabolism makes them vulnerable to harm.
The kidneys too play a central role in the metabolising of drugs, which predisposes them to considerable injury.
The function of both the liver and the kidneys in drug metabolism is to convert drugs into substances called metabolites that are easier to dispose of.
Unfortunately, metabolites are often more toxic than the drug itself. This may cause cellular damage and ultimately lead to organ dysfunction.
For example, a commonly prescribed pain killer called Tramadol is converted to a metabolite called O-desmethyl-tramadol in the liver, which is up to 4 times more potent than tramadol itself.
Metabolism of morphine in the liver and kidneys has been associated with toxic liver damage and deterioration of kidney function.
For help overcoming opioid addiction, call us today on 0800 140 4690
Cocaine is an addictive stimulant drug derived from the Erythroxylum coca plant native to South America.
Cocaine blocks the reuptake of three chemical messengers called dopamine, serotonin, and norepinephrine, thus enhancing the duration and intensity of its short-term effects.
Some short-term effects of cocaine include:
Although pharmacologically different from opioids, cocaine is similar to opioids in the sense that it is a powerful reinforcer and motivates continued use to satisfy cravings.
Despite the mostly pleasurable short-term effects of cocaine, continued abuse can lead to a range of harmful long-term effects which may include:

Having excess levels of dopamine in the brain over a prolonged period can cause structural damage, which may ultimately lead to the development of life-threatening medical conditions.
Like alcohol, cocaine abuse can lead to reductions in gray and white matter.
One study on people who were either addicted to cocaine or had used cocaine in the last year, reported a 50% reduction in grey matter in the brains of participants.
These findings suggest that cocaine abuse may be responsible for memory and mood deficits, as well as reduced ability to regulate emotions. This may accelerate the ageing process.

Cocaine is one of the most important risk factors for stroke in adults, particularly young adults. The neurotoxic effects of cocaine can cause both ischaemic strokes and hemorrhagic strokes.
Interestingly, abuse of cocaine in powdered form is more likely to result in hemorrhagic strokes, while smoking crack cocaine results in equal numbers of both ischaemic and hemorrhagic strokes.
Stroke caused by cocaine abuse can lead to toxin-associated seizures that may be life-threatening.
People with pre-existing epilepsy are more likely to sustain cocaine-related seizures.

Cocaine abuse can accelerate the onset of pre-existing movement disorders and has been associated with involuntary movement disorders in people without a predisposition.
Furthermore, cocaine abuse can aggravate the symptoms of movement disorders like Tourette’s syndrome, tremors, and dystonia, and may cause a return of these disorders in people who had been in remission.

The main complaint for the majority of patients who present themselves at emergency departments in the aftermath of cocaine abuse is chest pain.
Cocaine puts immense stress and pressure on the heart muscles because it increases the amount of oxygen the heart requires but restricts oxygenated blood flow.
In people under the age of 50, cocaine abuse is the biggest risk factor for cardiac death.
The scientific literature on cocaine-related cardiac complications suggests that adults who die from sudden cardiac death are up to 4 times more likely to have recently abused cocaine.

It is also important to note that most people who consume cocaine do so when they are under the influence of alcohol.
The combination of alcohol and cocaine applies up to 30% extra stress, on the heart on top of the considerable stress caused by consuming either one of these drugs alone.
Cocaine abuse may also cause the following long-term cardiovascular complications:

The rising use of cocaine worldwide has caused a significant increase in the prevalence of medical complications related to intranasal ingestion (snorting) of the drug.
Cocaine’s corrosive effect on blood vessels can cause a reduction in blood flow which may ultimately lead to the development of small holes called perforations.
Nasal perforations can have a range of side effects, including dry nose, blocked nose, crusting, bleeding, scabbing, and headache.
Snorting cocaine can also cause perforations in the roof of the mouth and nasal septum, as well as the collapse of the nasal cavity and deformation of the upper jaw.
To find the ideal drug rehab for treating your cocaine addiction, call us on 0800 140 4690

Like cocaine, methamphetamine is a highly addictive central nervous system stimulant drug that blocks the reuptake of dopamine, serotonin, and norepinephrine.
As a result, methamphetamine use mimics the effects of the sympathetic nervous system, producing feelings of euphoria and alertness, and elevating mood.
Methamphetamine can come in a variety of different forms, and as a consequence, can be smoked, injected, snorted, or orally ingested.
The most popular method of using methamphetamine is by smoking its hydrochloride salt form, which is mostly referred to as crystal meth.
Scientific evidence suggests that methamphetamine is the third most harmful drug of abuse to individuals.
Long-term effects of methamphetamine abuse may include:

Continued abuse of methamphetamine can cause long-term brain injury.
Binging on methamphetamine can produce long-lasting reductions in dopamine and serotonin, chemicals that are central to feelings of pleasure and the regulation of mood.
Methamphetamine abuse is associated with many markers of cognitive decline, including deficits in memory, attention, and decision-making.
One study examining the cognitive function of current abusers of methamphetamine showed impairments in recognition and recall of words and pictures, information processing speed, selective attention, and abstract thinking.

Abuse of methamphetamine over a prolonged period of time may cause psychosis characterised by auditory and visual hallucinations, false memories, and paranoid delusions.
In fact, reports of methamphetamine-induced psychosis are common in certain parts of the world.
People with methamphetamine-induced psychosis are significantly more likely to be diagnosed with co-morbid disorders such as depression, alcohol use disorder, and antisocial personality disorder than the general population.
It is thought that depression may be common among methamphetamine-addicted persons due to challenging symptoms associated with methamphetamine withdrawal, or the sub-optimal conditions of the addictive lifestyle.

Methamphetamine abuse can accelerate the onset of psychosis in people with a genetic predisposition to schizophrenia.
Abuse of methamphetamine in conjunction with alcohol consumption has also been shown to exacerbate disorders like schizophrenia and depression.
A Japanese study on people formerly addicted to methamphetamine reported that symptoms of psychosis may persist for years after withdrawal.
14% of the patients in this study remained in the hospital for over 5 years post-withdrawal.
Similarly, a study done in Australia found that people with an addiction to methamphetamine were 3 times more likely to have experienced psychotic symptoms than their non-addicted methamphetamine users.
Furthermore, the prevalence of psychosis among methamphetamine abusers was 11 times higher than the general population.

Like other central nervous stimulant drugs, methamphetamine can have seriously harmful and potentially deadly effects on the cardiovascular system.
Methamphetamine abuse puts people at greater risk of cardiac pathology and consequential cardiac events.
The most common symptoms that people present with at emergency departments after a methamphetamine overdose are chest pain, hypertension, arrhythmia and palpitations.
Chronic abuse of methamphetamine can lead to chronic hypertension which increases the risk of suffering a heart attack, stroke and heart failure.
Regarding the relationship between methamphetamine abuse and sudden cardiac death, it is important to note that even relatively small doses of methamphetamine can cause sudden cardiac death in people who might be hypersensitive.

The most common cardiac complications associated with methamphetamine abuse that lead to death are acute heart attack, sudden cardiac death, and dissection of the body’s biggest artery, the aorta.
One study found methamphetamine abuse to be the second most common risk factor for fatal aortic dissection.
Methamphetamine is also associated with other serious cardiovascular complications including:
Beat your methamphetamine addiction by reaching out to our experts on 0800 140 4690

Deaths in which drug poisoning is an underlying cause account for approximately 36% of all drug-related deaths.
In 2017, more than 70,000 people died from an overdose in the U.S.
Aside from drug poisoning, there are other ways in which drug use increases the risk of dying that are not always sufficiently considered.
In addition to drug overdose, other causes of death among people addicted to drugs include:

A recent study which investigated more than a decade of deaths in the U.S. in people aged 15 and older indicated that drug-related mortality rates are highest between ages 25 and 59, while rates are lowest below age 20 and above age 65.
Furthermore, drug-related mortality appears to peak in the early 30s for men, and in the early 50s for women.
It is predicted that without the contribution of drug use to death rates, life expectancy at age 15 would improve by half a year in men, from 63.1 to 63.6 years. Among women, it is predicted that life expectancy would increase by 0.4 years, from 67.5 to 67.9 years.
It is estimated that in general, drug-related mortality costs men 1.4 years of life, and costs women 0.7 years of life. In some areas, drug use costs men 3.6 years of life, and costs women up to 1.9 years of life.
This impact on life expectancy displays the magnitude of problems associated with drug abuse.
Don’t let drug abuse take control of your life – get help from a drug and alcohol rehab suited to your needs by calling us on 0800 140 4690